Cancer is often talked about as one disease, but it’s actually hundreds of diseases, each with unique mutations, behaviours and responses to treatment. This is especially true for high-grade gliomas (HGG), aggressive brain tumours that cause the greatest loss of life among children and young adults. Many of these tumours originate from low grade gliomas (LGG) which remain stable for years before transformation into deadly gliomas (HGG) that current therapies can’t cure.
“Our team has identified the specific low-grade gliomas that will transform,” explains Dr. Uri Tabori, lead investigator of a new $3-million Terry Fox New Frontiers Program Project Grant and senior scientist at the Hospital for Sick Children (SickKids) in Toronto. “But we don’t yet have the tools to detect these tumours early, or the targeted immune treatments to stop them before they progress.”
With new funding from the Terry Fox Research Institute, the team is developing better tools to do both: detect high-risk brain tumours earlier and eliminate them using the body’s own immune system, before they become life-threatening.
A new vision for cancer interception
The multidisciplinary team calls this approach cancer interception. In other words, identifying high-risk gliomas early and treating them while they’re still “young and simple.”
“The best way to treat cancer is to prevent it,” says Dr. Tabori. “But because we can’t do that yet, the next-best thing is to intercept it early.”
This represents a major shift in how brain cancer is treated. Instead of waiting to see if gliomas will transform and then relying on toxic – often ineffective – therapies like radiation or chemotherapy, the team wants to intervene sooner with targeted, less harmful therapies that match each type of tumour.
“You wouldn’t use the same tactics to win at chess as you would in basketball,” says Dr. Tabori. “Immunotherapies are the same. We need to choose the right strategy based on each tumour’s biology.”
This personalized approach is especially important in brain cancer, where preserving healthy brain tissue is critical. Treatments must be effective but also safe, particularly for developing brains.
Innovative tools to catch cancer earlier
The team at SickKids will first work to improve early detection. Dr. Peter Dirks will study how inflammation and the immune system influence tumour development, and how the immune environment around tumours contributes to their transformation into HGG.
Dr. Cynthia Hawkins will uncover early warning signs that can immediately guide treatment decisions. Dr. Hawkins will also use non-invasive liquid biopsies – tests of blood or spinal fluid – in hopes of detecting these signals, or genetic markers, long before tumours transform.
Next, Dr. Adrian Levine will apply cutting-edge technologies to uncover vulnerabilities in gliomas, enabling Dr. Tabori and Dr. Anirban Das to design more effective immune therapies that target these vulnerabilities. Finally, Dr. James Rutka will bypass the blood-brain barrier to ensure these new therapies are delivered directly into the brain.
They will test these therapies in lab models and animal studies, with the ultimate goal of finding treatments that are effective across multiple types of high-grade gliomas.
“This kind of work requires collaboration of experts across many fields,” says Dr. Tabori. “It’s only through teamwork that we can translate discoveries into clinical care, ensuring kids in Canada have free access to the best possible care.”
New hope for children, and beyond
While the project focuses on children and young adults, the impact could extend much further. Because childhood cancers tend to be genetically simpler than those in adults, they offer a unique opportunity to create therapies that could then be applied more broadly.
“The leap between interception and prevention is very small,” says Dr. Tabori. “If we can eliminate young cancers before they transform, we may be able to stop them from forming in the first place.”
Thanks to the team’s existing partnership with Dr. Julie Bennet (SickKids) who co-leads the Canadian AYA Neuro-Oncology Network (CANON), any successful discoveries can be quickly translated into trials.
“Twenty years ago, every child was treated the same way. Our tools were limited, and outcomes were poor,” says Dr Tabori. “Now, we can personalize treatment. Every discovery brings us closer to giving kids not just survival, but a chance to laugh, play and thrive. As a researcher and clinician, this is what I dream of at night – and today, sometimes these dreams come true.”
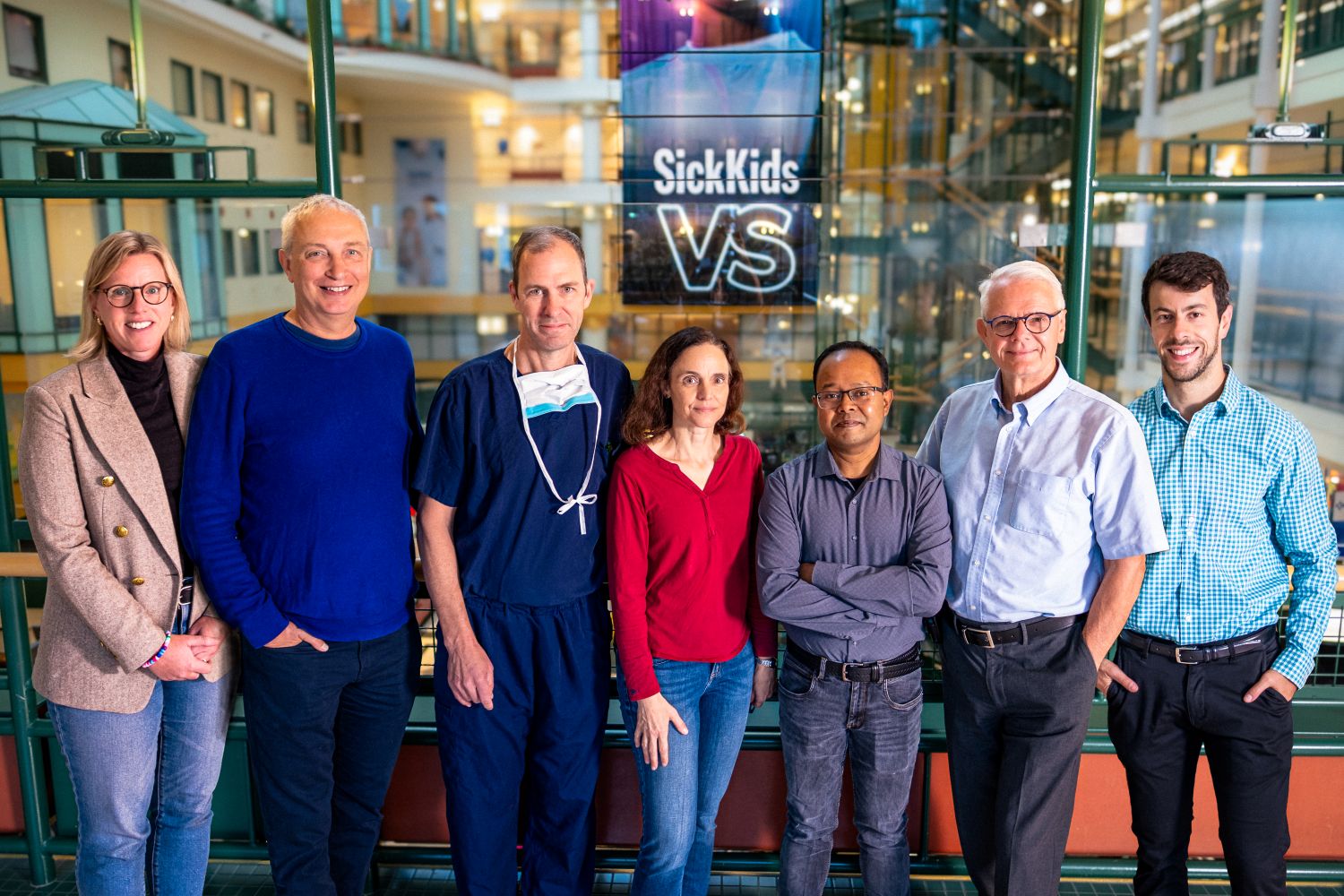
Terry Fox New Frontiers Program Project Grant team studying high-risk brain tumours (gliomas), led by Dr. Uri Tabori.