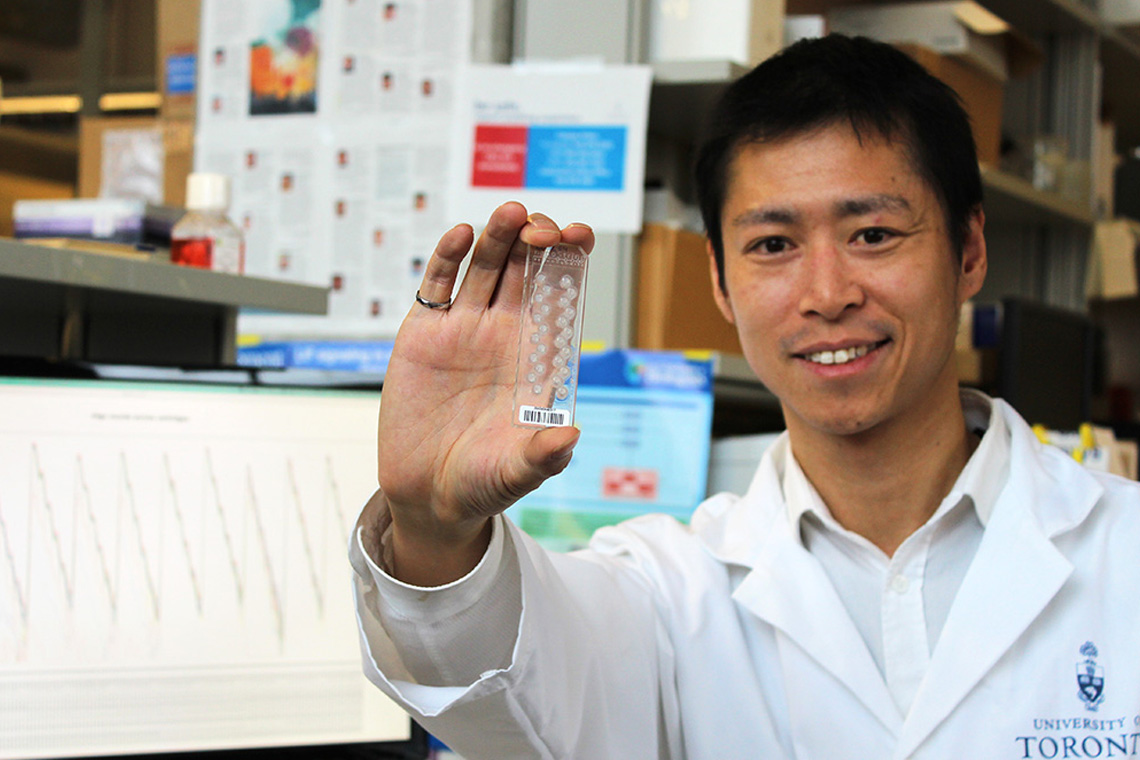
Researcher Stanley Ng holds up a cartridge used to measure the gene expression levels of cancer cells. (Photo: University of Toronto).
What if there was a way to predict if leukemia patients would respond to standard treatment or not? A TFRI-funded team has developed a novel, 17-gene signature test from leukemia stem cells (LSCs) that determines just that.
The test provides doctors with a risk scoring tool that can predict within just a day or two of diagnosis an acute myeloid leukemia (AML) patient’s treatment response, as well as aid clinicians in treatment decisions. The work was published in Nature (December 2016, first author Stanley Ng).
Patients predicted not to benefit from standard treatment could be guided to novel clinical therapies and/or post-remission strategies, according to the study’s lead investigator Dr. Jean Wang at Princess Margaret (PM) in Toronto.
AML is the deadliest form of leukemia, with low cure rates especially in older patients. Although many patients respond to initial therapy, disease recurrence is common and difficult to treat. The high rate of relapse in AML has been attributed to the persistence of LSCs, which possess numerous stem cell properties connected with treatment resistance.
The new biomarker, named the LSC17 score, is a signature of 17 genes that are specific to LSCs. To create it, the team first generated a list of genes differentially expressed between 138 LSC+ and 89 LSC− cell fractions derived from 78 AML patient samples. They then performed a sparse regression analysis of LSC gene expression against survival in a large training cohort.
Calculating a patient’s score is simple: the patient’s blood or bone marrow sample is tested to measure the expression levels of the 17 genes. Those with a higher LSC17 score have the greatest risk of death if treated with standard chemotherapy, knowledge that could guide clinicians to offer them alternative options such as a clinical trial.
Dr. John Dick, who leads TFRI’s prolific cancer stem cell program, was one of the co-senior authors of the team. Besides AML, Dr. Dick is also investigating the role of cancer stem cells in glioblastoma and multiple myeloma, two deadly and incurable cancers.
Study: A 17-gene stemness score for rapid determination of risk in acute leukemia
Authors: Stanley W. K. Ng, Amanda Mitchell, James A. Kennedy, Weihsu C. Chen, Jessica McLeod, Narmin Ibrahimova, Andrea Arruda, Andreea Popescu, Vikas Gupta, Aaron D. Schimmer, Andre C. Schuh, Karen W. Yee, Lars Bullinger, Tobias Herold, Dennis Görlich, Thomas Büchner, Wolfgang Hiddemann, Wolfgang E. Berdel, Bernhard Wörmann, Meyling Cheok, Claude Preudhomme, Herve? Dombret, Klaus Metzeler, Christian Buske, Bob Löwenberg, Peter J. M. Valk, Peter W. Zandstra, Mark D. Minden, John E. Dick & Jean C. Y. Wang.
Funding: This work was supported in part by the Terry Fox Foundation.
TFRI Links, Spring 2017